Abstract
Many therapies are available for trigeminal neuralgia (TN), from medical therapy to invasive, mininvasive and non-invasive methods. There is no a unique indication concerning the choice of treatment; we report our indications for gasserian ganglion compression with balloon by percutaneous approach.
Out of 421 patients affected by TN treated with various methods from 2004 through to 2014, we present 46 patients treated by gasserian ganglion compression with balloon catheter. Patients selected for this procedure were only those refractory to medical therapy and refractory to the other available therapies (radiofrequency, microvascular decompression, radiosurgery, glycerolization, peripheral alcoholizations): balloon compression was performed as third line therapy.
After the procedure, twenty-eight patients were classified as BNI pain intensity score grade 1, seven other as grade 2, three other as grade 3, six were classified as BNI grade 4, and in one patient no improvement of pain occurred (BNI grade 5). After an average period of follow up of 8,6 years, four cases of pain recurrence occurred.
Because balloon compression is an ablative and non-selective procedure and all three trigeminal divisions are damaged to achieve stable pain remission, the procedure was performed only in patients affected by recurrent TN refractory to the other available methods.
Author Contributions
Academic Editor: Farah Yousef, Damascus University, Syria.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2019 Mario Francesco Fraioli, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Trigeminal neuralgia (TN) is a social disabling disease and nowadays still represents a therapeutic challenge 1, 2, 3. In general, many therapeutic options are available for TN, from invasive (microvascular decompression 4, mininvasive 5, 6, 7, 8, 9 and non invasive (Radiosurgery/Hypofractionated radiotherapy 10, 11, 12 ones. Usually, medical therapy with carbamazepine represents the first therapeutic choice 13 and when it is ineffective or patients are intolerant, the above-mentioned methods are employed.
Based on the available literature, when medical therapy is ineffective, it is evident that the choice between the various therapeutic methods is not well established, and it depends mainly from operator’s familiarity with one or another technique and from the technological devices available in the center where the patient is referred to. We observed that only few authors 3, and only partially, selected one or another procedure according to patients (advanced age, medical conditions) and neuralgia (trigeminal division, gravity of neuralgia) characteristics. Concerning 421 patients affected by trigeminal neuralgia refractory to medical therapy treated with various methods from 2004 through to 2014 in our centres, we present 46 patients treated with gasserian ganglion compression with balloon catheter.
Materials and Methods
Selection of patients to perform gasserian ganglion compression with balloon catheter was based according to: interested trigeminal division, severity of neuralgia, previous treatments.
Procedure was performed in day-surgery (22 patients) and with 24 hours hospitalization (24 patients), under fluoroscopic control, in sedation without necessity of general anesthesia.
Results concerning postoperative pain were analyzed according to Barrow Neurological Institute Pain Intensity Score (Table 1).
Table 1. Barrow Neurological Institute Pain Intensity Score| Score | Pain description |
|---|---|
| 1 | No pain, no medications |
| 2 | Occasional pain, no medications required |
| 3 | Some pain, adequately controlled with medications |
| 4 | Some pain, not adequately controlled with medications |
| 5 | Severe pain or no pain relief |
Postoperative controls, to evaluate efficacy of the procedure, was conducted one day, 10 days and 4 weeks after treatment; after one month, if no results have been achieved, treatment was considered failed.
Procedure of gasserian ganglion compression with balloon catheter is an ablative and non-selective procedure, which has the objective to damage gasserian ganglion by compression; consequently, all three trigeminal divisions are damaged to achieve pain remission: the effect is a various degree of hypoesthesia of the entire hemifacial side.
Ten patients were affected by first division (V1) TN (Table 2), since an average period of 10,5 years; average age of patients was 74 years; neuralgia had been refractory to multiple therapies performed both in our Institution and in other Institutes, therapies represented by radiosurgery performed in all patients and repeated in 3 of them, peripheral alcoholizations in all patients repeated in 2 cases, microvascular decompression in 3 patients, glycerolization in one patient.
Table 2. Previous treatments performed by 10 patients affected by first division (V1) TN| Patient | Age | Medical conditions | Lenght of clinical history (years) | Previous treatments |
| 1 | 66 | Good | 4,5 | PA, MVD, RS(2), |
| 2 | 58 | Good | 6,7 | RS, PA(2) |
| 3 | 78 | Poor | 7,8 | PA, RS |
| 4 | 89 | Poor | 12,2 | RS, PA, GLY |
| 5 | 88 | Poor | 10,4 | PA, RS |
| 6 | 72 | Poor | 9,5 | PA(2), RS |
| 7 | 69 | Poor | 2,7 | MVD, RS(2), PA |
| 8 | 86 | Poor | 8,6 | PA, RS |
| 9 | 69 | Poor | 8,2 | RS(2), PA |
| 10 | 65 | Good | 4,3 | MVD, RS, PA |
Twelve patients were affected by second division (V2) TN (Table 3), since an average period of 9,5 years; average age of patients was 66,6 years. Previous treatments had been performed: peripheral alcoholizations in all patients (repeated once in 4 cases), stereotactic radiosurgery in all patients (repeated once in 3 cases), microvascular decompression in 3 patients and glycerolization (performed in other Institutes) in 3 other patients.
Table 3. Previous treatments performed by 12 patients affected by second division (V2) TN| Patient | Age | Medical conditions | Lenght of clinical history (years) | Previous treatments |
| 1 | 52 | Good | 4,5 | PA, MVD, RS(2), |
| 2 | 67 | Good | 6,7 | RS, PA(2) |
| 3 | 76 | Poor | 7,8 | PA, RS |
| 4 | 90 | Poor | 12,2 | RS, PA, GLY |
| 5 | 83 | Poor | 10,4 | GLY, PA, RS |
| 6 | 81 | Poor | 9,5 | PA(2), RS |
| 7 | 57 | Poor | 2,7 | MVD, RS(2), PA |
| 8 | 76 | Poor | 8,6 | PA(2), RS |
| 9 | 78 | Poor | 8,2 | GLY, RS(2), PA |
| 10 | 59 | Good | 4,3 | MVD, RS, PA |
| 11 | 90 | Poor | 9,8 | PA(2), RS |
| 12 | 72 | Good | 6,9 | PA, RS |
The last 24 patients (Table 4) were affected by V1 and V2 TN; average age was 74,9 years; average length of clinical history was 9 years. Previous treatments were represented by radiosurgery in all patients repeated once in 6 patients, peripheral alcoholizations in all patients repeated once in 5 patients and twice in 2 cases, microvascular decompression in 8 patients, glycerolization in 4 ones.
Table 4. Previous treatment performed by 24 patients affected by V1 and V2 trigeminal neuralgia PA = peripheral alcoholizations; RS = radiosurgery; MVD = microvascular decompression; GLY = glycerolization Number in bracket indicates the total number of procedures performed in the related patient| Patient | Age | Medical conditions | Lenght of clinical history (years) | Previous treatments |
| 1 | 66 | Good | 6,7 | PA(2), MVD, RS |
| 2 | 78 | Poor | 9,2 | PA, RS, GLY |
| 3 | 77 | Poor | 6,9 | GLY, PA, RS |
| 4 | 59 | Good | 3,6 | PA, MVD, RS(2) |
| 5 | 82 | Poor | 13,4 | PA(2), RS |
| 6 | 85 | Poor | 15,5 | GLY, PA, RS |
| 7 | 67 | Poor | 5 | PA, RS(2) |
| 8 | 73 | Good | 7,5 | PA(3), MVD, RS |
| 9 | 75 | Good | 8,1 | PA, MVD, RS(2) |
| 10 | 78 | Good | 9,4 | PA, RS |
| 11 | 81 | Poor | 12,1 | PA(2), RS |
| 12 | 80 | Poor | 15 | PA, RS |
| 12 | 56 | Good | 3,3 | PA, MVD, RS(2) |
| 14 | 73 | Good | 5,9 | PA(2), MVD, RS |
| 15 | 82 | Poor | 9,1 | PA, RS |
| 16 | 59 | Poor | 4,2 | PA, RS(2) |
| 17 | 61 | Good | 7,1 | PA, MVD, RS |
| 18 | 63 | Poor | 5,5 | PA(3), RS |
| 19 | 90 | Poor | 15,1 | PA, RS |
| 20 | 85 | Poor | 14,7 | GLY, PA, RS |
| 21 | 67 | Good | 5,7 | PA, MVD, RS(2) |
| 22 | 77 | Poor | 9 | PA , RS |
| 23 | 81 | Good | 7,8 | PA(2), RS |
| 24 | 88 | Poor | 16,7 | PA, RS |
Selection of Patients
As above reported 7, balloon compression leads to entire hemifacial hypoesthesia with no possibility to select in particular one trigeminal division/hemifacial district, differently from the other ablative procedures as radiofrequency thermocoagulation and peripheral alcoholizations which allow to achieve selective anesthesia in a single trigeminal division/facial district. Because entire hemifacial hypoesthesia is not well tolerated by the patients than hypoesthesia/anesthesia in only one trigeminal division which is, on the contrary, usually well tolerated, patients selected for this procedure were only those affected by TN refractory to all the other procedures (radiosurgery, glycerolization, peripheral alcoholizations, microvascular decompression when indicated). Therefore, balloon compression was never used by us as second therapeutic method to treat TN refractory to medical therapy. Moreover, thanks to the well-known efficacy of radiofrequency thermocoagulation for third division (V3) TN 14, balloon compression was never employed by us for patients affected by isolated V3 TN.
Procedure of Balloon Cmpression
Under fluoroscopic control, in deep sedation without endotracheal intubation, a 4-F balloon catheter with a capacity of 0,7 ml was inserted into the foramen ovale through a 12 gauge teflon catheter guide (Figure 1). The balloon was conducted into the Meckel cave and fluoroscopic control was performed; at this point, the balloon was inflated with iopamidol generating compression of gasserian ganglion (Figure 2); the balloon was kept in situ inflated, compressing the ganglion for about 3-4 minutes. After this time, balloon was deflated but kept into the Meckel cave and sedation was suspended to test the patient: facial sensitivity was explored and procedure was concluded if hypoesthesia was achieved. In 6 patients level of hypoesthesia was too weak, so that patient was sedated again and balloon was inflated and kept is situ for other 6 minutes; suspended sedation, in all patients hypoesthesia was satisfactory and procedure was concluded. Sizes of inflated balloon were: length 18 mm, diameter 6 mm, volume of inflation 0,7 cc.
Figure 1.Procedure of gasserian balloon compression under fluoroscopic control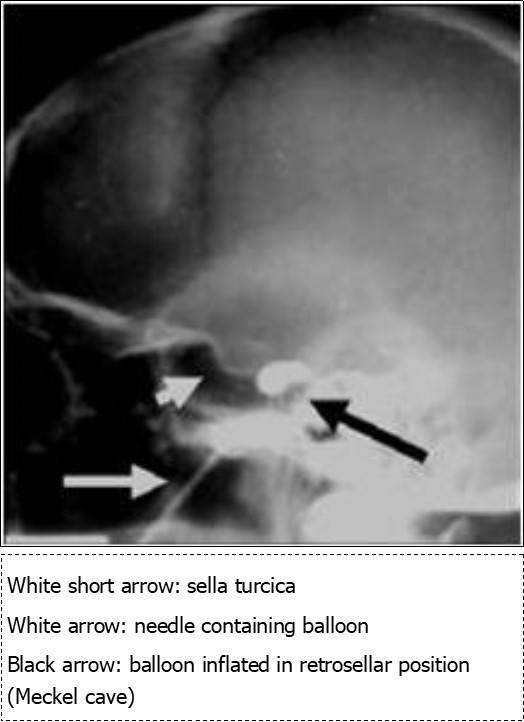
Figure 2.A: needle positioning into the Meckel cave (retrosellar position)
Results
Differently from other ablative techniques such as radiofrequency thermocoagulation 14 and peripheral alcoholizations 7, after which pain control is immediate after the procedure, remission of trigeminal pain after balloon compression was observed after an average period of 8,9 days; therefore, all patients were evaluated 1 day after procedure, after 1 week and after 1 month. One month after the operation we observed no changes of pain status in any patients. In no patient anesthesia dolorosa occurred. In 3 patients weakening of corneal reflex occurred with necessity of ocular protection (glasses for outdoor), eye drops, etc. Four patients presented masseter muscle weakness and three other presented cheek hematoma. Only one patient showed intolerance to hemifacial hypoesthesia, although pain remission occurred.
Pain Remission and Hemifacial Sensitivity
Out of 46 patients submitted to balloon compression, thirty-nine (84,8%) presented pain remission within one month; concerning these patients, medical therapy was suspended in 35 (BNI pain intensity score grade 1 in 28 patients, grade 2 in 7), while it was maintained with low dosage of carbamazepine and oxcarbazepine respectively in 3 and 1 patients (BNI pain intensity score grade 3). Out of the other 7 patients, six presented some pain although they continued medical therapy and they were classified as BNI pain intensity score grade 4; in the last patient we registered no pain relief (BNI pain intensity score grade 5).
Regarding hemifacial sensitivity, final result was evaluable within 1 month; in no patient complete hemifacial anesthesia was observed. Twenty-three patients presented marked hemifacial hypoesthesia after the procedure, which corresponded to immediate pain remission, and it remained unchanged during the follow-up (9,2 years) in all patients but 2 who presented recovery of facial sensitivity and recurrence of trigeminal pain after 5,4 and 7,2 years. Seventeen patients presented slight hemifacial hypoesthesia immediately after the procedure, with only slight improvement of dolorific attacks; during postoperative days (4-28 days), level of hemifacial hypoesthesia progressively increased with concomitant improvement of dolorific attacks; high grade of facial hypoesthesia remained unchanged during follow-up (7,2 years) in all patients but 2 who presented pain recurrence after 3,4 and 6,2 years, at the same time with recovery of hemifacial sensitivity. Five other patients presented only slight hemifacial hypoesthesia after the procedure, immediate after the procedure in 3 cases and after a period of 18 and 29 days in the other 2 cases respectively; all these patients presented only minimal result concerning pain control (classified as grade 4 of BNI pain intensity score). The last patient in whom no hypoesthesia was achieved, presented no result concerning pain control: both facial sensitivity, and trigeminal pain remained unchanged (BNI grade 5)
Recurrence and treatment
After an average period of follow up of 8,6 years after procedure, we observed 4 cases of pain recurrence; in all these patients, recurrence of pain corresponded to recovery of facial sensitivity. Recurrence was not related to the previous BNI pain score intensity after first procedure of ganglion compression. Three of them were treated with new procedure of balloon compression, achieving a satisfactory level of hemifacial hypoesthesia and remission of pain. In the last patient, originally affected by first and second divisions TN, presenting recurrence of the only second division TN, the same procedure was attempted, but it was not possible to insert the balloon into the Meckel cave, probably because of fibrosis due to the previous procedure; the patient was then treated with surgical infraorbital (maxillary) nerve avulsion.
Discussion
The main problem concerning the treatment of trigeminal neuralgia refractory to medical therapy is the following: it is better to select percutaneous mininvasive therapy which present a very low rate of complicances, a very high rate of pain control but facial sensitive deficit? Or to select major interventions, which present major rate of complicances, but high rate of success with facial sensitivity sparing? Or it is better to employ non invasive therapy (radiosurgery), with ineligible rate of risk/complicances, very high rate of facial sensitivity sparing but inferior rate of pain control than the other procedures? We retain that there is no answer to this question, therefore patients should be carefully selected for any kind of therapy, avoiding to perform one or another procedure according only to operator familiarity with one single procedure. Therefore, because balloon compression is a non selective procedure which operates compressing the entire ganglion producing damage to all three trigeminal divisions (with consequent entire hemifacial hypoesthesia), it was never used by us as first therapeutic method to treat TN refractory to medical therapy, but it was employed only for recurrence after other previous therapies.
Concerning balloon compression, only few authors 3 reported criteria of selection of patients for this procedure: they reported that balloon compression was used in particular for patients affected by V1 TN instead of radiofrequency thermocoagulation, because the second caused a very high rate of corneal reflex deficit; moreover, they reported that balloon compression was proposed for patients with acute neuralgia in place of radiosurgery because of the necessity of immediate pain relief, because it is well known that effect of radiosurgery occurs after several weeks 12.
Pain Remission / Level of Hypoesthesia
Putting in relationship the level of hemifacial hypoesthesia and the level of postoperative pain remission, we observed that the best results were achieved in patients presenting postoperative high degree of hypoesthesia (BNI 1 e 2) as observed in our previous series of patients treated with other ablative percutaneous procedures 7, 14. In patients presenting only slight postoperative hypoesthesia, control of pain was lower than the previous (BNI 3 and 4); some authors 15 reported a very low rate of postoperative facial dysesthesia/hypoesthesia, but a very high rate of pain recurrence; in this way, balloon compression could be considered a procedure able to achieve only temporary pain remission. No improvement of pain was observed in the only one patient of our series in whom no hypoesthesia was achieved. Therefore, we can conclude that, as well as with the other percutaneous ablative techniques in our experience, hemifacial hypoesthesia is necessary to achieve satisfactory results concerning pain remission (BNI 1 and 2). Many Authors consider facial hypoesthesia a complication 2, 9, 16, and the low rate of facial hypoesthesia reported from these authors corresponded to a high rate of pain recurrence after a relatively short time and in not few cases some authors considered balloon compression as a temporary procedure. Only few Authors 17 reported that hemifacial dysesthesia/hypoesthesia is a quite unavoidable effect associated to a successful operation.
The period of time necessary to produce hypoesthesia, variable from immediate postoperative period to 28 days in our experience, did not result a significant prognostic factor concerning postoperative control of pain or concerning pain recurrence.
Only one patient presented intolerance to hemifacial hypoesthesia, while the other accepted without any problem the sensitive deficit necessary to achieve pain remission. This is a very important aspect that proves that a strict selection of patients and clear preoperative explanation of the procedure and its effects is necessary.
Reason because different hypoesthesia is achieved in different patients, mainly concerns position of the balloon into the Meckel cave and overall the atrophic or non-atrophic condition of the ganglion; in other words, when ganglion is atrophic, Meckel cave is in part empty, as it occurs for example in “empty sella”, and compression with balloon is less efficacious because of the empty space.
Timing of hypoesthesia
Ganglion compression causes ischemic damage and this fact leads to pain remission. Differently from radiofrequency thermocoagulation in which pain remission is immediate and related to immediate postoperative anesthesia/hypoesthesia in V3, balloon compression caused hemifacial sensitivity modifications until 28 days after the procedure in not few patients (seventeen) of our series compared to the immediate postoperative result. This is a clear indication that ischemic lesion occurred progressively after balloon compression in several patients.
Conclusions
In conclusion,percutaneous gasserian ganglion balloon compression resulted a safe and efficacy procedure. Because this is an ablative and non-selective procedure and all three trigeminal divisions are damaged to achieve stable pain remission, the procedure was performed only in patients affected by recurrent TN refractory to the other available methods.
References
- 1.Miller J P, AcarF BurchielKJ. (2009) Classification of trigeminal neuralgia: clinical, therapeutic, and prognostic implications in a series of 144 patients undergoing microvascular decompression. doi: 10.3171/2008.6.17604.J Neurosurg.111(6):. 1231-4.
- 2.Abdennebi B, Guenane L. (2014) Technical considerations and outcome assessment in retrogasserian balloon compression for treatment of trigeminal neuralgia. Series of 901 patients. Surgical Neurology International 5-118.
- 3.Noorani I, Lodge A, Vajramani G, Sparrow O. (2016) Comparing Percutaneous Treatments of Trigeminal Neuralgia: 19 Years of Experience in a Single Centre. , Stereotact Funct Neurosurg 94, 75-85.
- 4.Feng BH1,Zheng XS,Liu M,Wang XQ,Wang XH, et al. (2015).Microvascular Decompression for Trigeminal Neuralgia:Zone Exploration and Decompression Techniques.JCraniofacSurg.26(8):. 2381-4.
- 5.Asplund P, Blomstedt P, Bergenheim A T. (2016) Percutaneous Balloon Compression vs Percutaneous Retrogasserian Glycerol Rhizotomy for the Primary Treatment of Trigeminal Neuralgia doi: 10.1227/NEU.0000000000001059. , Neurosurgery 78, 421-428.
- 6.Cheng J S, Lim D A, Chang E F, Barbaro N M. (2014) A Review of Percutaneous Treatments for Trigeminal Neuralgia DOI: 10.1227/NEU.00000000000001687. , Operative Neurosurgery 10, 25-33.
- 7.Fraioli M F, Lecce M, Lisciani D, Fraioli B. (2011) Trigeminal Neuralgia: Role and Neurosurgical Indications of Peripheral Alcohol Injections, Controlled Radiofrequency Thermocoagulation, Gasserian Ganglion Compression with Balloon and Microvascular Decompression in Posterior Cranial Fossa. Experience in 437 Patients. , doi.org/10.4172/2155-9562.1000109 J Neurol Neurophysiol 2, 1.
- 8.Missios S, Mohammadi A M, Barnett G H. (2014) Percutaneous Treatments for. , Trigeminal Neuralgia Neurosurg doi.org/10.1016/j.nec.2014.06.008 Clin N Am 25, 751-762.
- 9.Yadav S, Sonone R M, Jaiswara C, Bansal S, Singh D. (2016) Long-term Follow-up of Trigeminal Neuralgia Patients treated with Percutaneous Balloon Compression Technique: A Retrospective Analysis The. , Journal of Contemporary Dental Practice 17(3), 263-266.
- 10.J1 Cohen, Mousavi S H, Faraji A H, Akpinar B, Monaco E A. (2017) . Stereotactic Radiosurgery as Initial Surgical Management for Elderly Patients with Trigeminal Neuralgia. doi: 10.1159/000468526 Stereotact Funct Neurosurg 95(3), 158-165.
- 11.Fraioli M F, Strigari L, Fraioli C, Lecce M, Lisciani D. (2012) Preliminary results of 45 patients with trigeminal neuralgia treated with radiosurgery compared to hypofractionated stereotactic radiotherapy, using a dedicated linear accelerator. , J Clin Neurosci 19(10), 1401-3.
- 12.Niranjan A, Lunsford L D. (2016) Radiosurgery for the management of refractory trigeminal neuralgia. doi: 10.4103/0028-3886.185393. , Neurol India 64(4), 624-9.
- 13.Cruccu G. (2017) Trigeminal Neuralgia. Continuum Minneap Minn, Selected Topics in Outpatient Neurology, doi: 10.1212/CON.0000000000000451. 23(2), 396-420.
- 14.Fraioli M F, Cristino B, Moschettoni L, Cacciotti G, Fraioli C. (2009) Validity of percutaneous controlled radiofrequency thermocoagulation in the treatment of isolated third division trigeminal neuralgia doi: 10.1016/j.surneu.2007.09.024. , Surgical Neurology 71, 180-183.
- 15.Martin S, Teo M, Suttner N. (2015) The effectiveness of percutaneous balloon compression in the treatment of trigeminal neuralgia in patients with multiple sclerosis doi: 10.3171/2014.11.JNS14736. , J Neurosurg 123(6), 1507-11.
